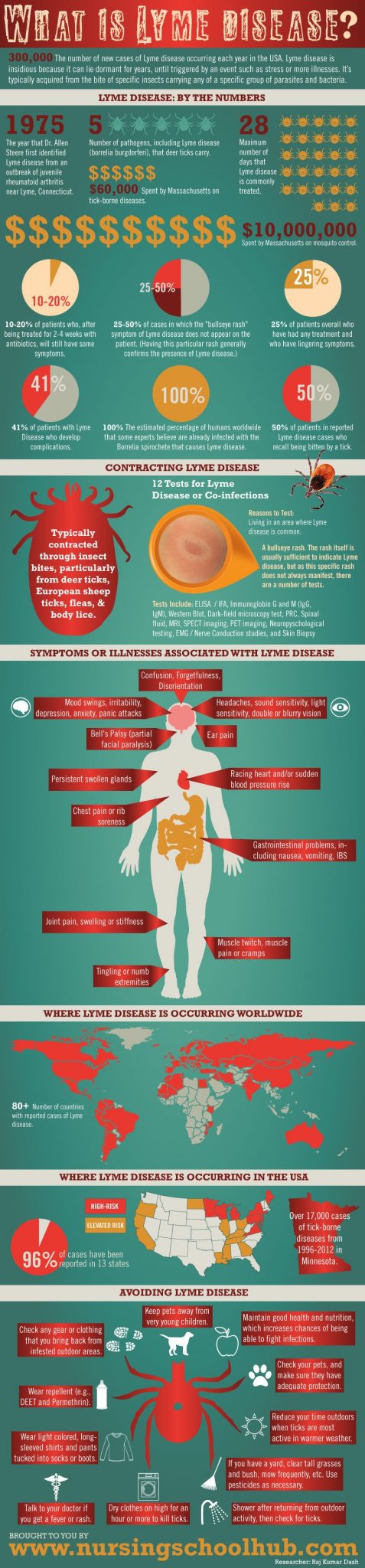
Lyme Disease infographic summarizes Lyme Disease contraction, symptoms, and treatment options for individuals who get it.
What is Lyme Disease?
The CDC recently published a scary statistic: 300,000. That’s the number of new cases of Lyme disease now occurring each year in the USA. That’s 10 times the CDC’s former estimate, and the reason it’s so scary is that Lyme disease is associated with 350 different health conditions. Lyme disease is insidious because it can lie dormant for years until a trigger event such as stress activates one or more illnesses.
Featured Programs
Lyme disease, typically acquired from the bite of specific insects carrying any of a specific group of parasites/ bacteria, often brings with it a variety of other illnesses or “co-infections”. This Lyme disease “complex” includes a number of documented illnesses, including Chronic Fatigue Syndrome (CFS, aka Epstein-Barr virus — once called by the media “Yuppie disease”) and possibly has a link to Fibromyalgia and other ailments.
When it does manifest, due to stress or deteriorating health, Lyme disease can bring with it around a dozen other co-infections. The difficulty for many sufferers is that not all nurses and medical professionals believe it exists, and many of those don’t know enough about it. It’s an illness for which there’s a short time window for effective treatment.
The Stats
- 1975 — The year that Dr. Allen Steere first identified Lyme disease from an outbreak of juvenile rheumatoid arthritis near Lyme, Connecticut.
- 1982 — The year that Willy Burgdorfer determined the etiological agent of Lyme disease — a type of spirochete of the genus Borrelia. Hence the name Borrelia burgdorferi for these spirochetes from Ixodes ticks.
- 300,000 — Number of Americans infected with Lyme disease each year, as per CDC reports. Roughly 0.01% of the population gets infected annually.
- 20,000 — The number of new cases reported in 2002.
- 30,000 — The number of new cases reported in 2009.
- 10 — The number of times higher that the actual number of Lyme disease cases is compared to what the CDC had previously estimated (300K compared to 30K).
- 28 — Maximum number of days that Lyme disease is commonly treated for.
- 10-20 — Percentage of patients who, after being treated for 2-4 weeks with antibiotics will still have some symptoms (fatigue, pain, joint and muscle aches. This is thought to be due to residual tissue and immune system damage.
- 25 — Percentage of patients overall who have had any treatment and who have lingering symptoms – usually for just a few days.
- 3-4 — The number of weeks after which, according to the CDC, antibiotic treatment is unlikely to lead to any patient improvement.
- 4-6 — The typical number of weeks of treatment. (Some insurance companies will not cover treatment past this time period, even though a patient may have residual spirochetes after treatment.)
- 5 — Number of pathogens, including Lyme disease (borrelia burgdorferi), that deer ticks carry.
- 350 — Number of diseases or illnesses that the co-infection Babesiosis mimics or cause. Other co-infections of Lyme (Borreliosis) disease include Bartonella, Ehrlichiosis (HME, HGE), Candida, Human Herpes Virus 6 (HHV-6), Epstein-Barr Virus (HHV-4, aka CFS or Chronic Fatigue Syndrome) and Cytomegalovirus (CMV). Babesia parasites can also trigger anemia, parasitaemia, and cardiovascular, kidney and liver problems.
- 50 — Percentage of patients who will suffer from seizures if they contract brain encephalopathy due to Bartonella coinfection.
- 100 — The estimated percentage of human beings worldwide who will at some point in their life be infected with the Epstein-Barr virus.
- 100 — The estimated percentage of humans worldwide that some experts believe are already infected with the Borrelia spirochete that causes Lyme disease.
- 30-45 — The number of days before symptoms of Epstein-Barr (chronic fatigue) will manifest.
- 80 — Estimated percentage of adults in the USA who are infected with Cytomegalovirus. CMV can stay dormant in the human host for the latter’s lifetime, and staying that way until the immune system is compromised.
- 41 — Percentage of patients who develop complications. These include acute respiratory failure, congestive heart or renal failure.
- 1-8 — Percentage of patients with Ehrlichiosis who die. This rate goes up drastically if the patient is immunocompromised.
- 13 — Percentage of Candida infections worldwide that have been identified.
- 25-50 — Percentage of cases in which the “bullseye rash” symptom of Lyme disease does not appear on the patient. (Having this particular rash generally confirms the presence of Lyme disease.)
- 50 — Percentage of patients in reported Lyme disease cases who recall being bitten by a tick.
- 40 — Percentage of cases in which spirochetes are actually seen. (The borrelia spirochete changes shape and can hide between blood cells when taken out of the host body.
- 4 — The number of combinations of infections typical in patients with chronic Lyme disease.
- 80+ — The number of countries where Lyme disease has been reported.
- 60,000 — The number of dollars spent by Massachusetts on tick-borne diseases (of which Lyme disease is the most prevalent).
- >10,000,000 — The number of dollars spent by Massachusetts on mosquito control
Ways to Get Lyme disease
Insect bites, particularly from Deer ticks, European sheep ticks, fleas, body lice.
Risk for Getting Lyme disease or Co-infections
The initial consideration for testing for Lyme disease includes:
- Living in an area where Lyme disease is common. (There are cases all over the US and Canada.)
- A bullseye rash (Erytherma migrans).
Tests for Lyme Disease
The rash itself is usually sufficient to indicate Lyme disease, but as this specific rash does not always manifest, there are a number of tests.
- ELISA (Enzyme-Linked Immunosorbent Assay) / IFA (Immunofluorescence assay)
- Immunoglobin G and M (IgG, IgM)
- Western Blot
- Dark-field microscopy test with silver nitrate stain
- PRC (Polymerase Chain Reaction)
- Spinal fluid
- MRI (Magnetic Resonance Imaging
- SPECT (Single Photon Emission Computerized Tomography) imaging
- PET (Positron Emission Tomography) imaging
- Neuropsychological testing.
- EMG (Electromyography) / Nerve Conduction studies
- Skin Biopsy.
8 Common Lyme disease-related co-infections
- Bartonella henselae (causes cat-scratch fever, endocarditis, and more).
- Epstein-Barr
- Cytomegalovirus (CMV)
- Babesiosis
- Human Herpes Virus 6 (HHV-6A and -6B)
- Ehrlichiosis (HME and HGE)
- Chlamydia pneumonia
- Candida
Associated symptoms or illnesses due to Lyme disease
- Muscle twitch, muscle pain, or cramps
- Racing heart
- Sudden blood pressure rise
- Tingling or numb extremities
- Headaches, sound sensitivity, light sensitivity, double or blurry vision
- Ear pain
- Bell’s Palsy (partial facial paralysis)
- Chest pain or rib soreness
- Persistent swollen glands
- Joint pain, swelling, or stiffness
- Confusion, difficulty in thinking; using the wrong words
- Forgetfulness, disorientation
- Mood swings, irritability, depression, anxiety, and panic attacks.
- Gastrointestinal problems, including nausea, vomiting, and IBS.
- Possible connections to Fibromyalgia (FMS), ADHD, anxiety disorder, bipolar disorder, insomnia, post-traumatic stress disorder, and more — because Lyme disease impacts the HPA (Hypothalamic-Pituitary-Adrenal Axis), and many of these illnesses are associated with HPA imbalance.
This is an incomplete list. Check Dr. Joseph Burrascano’s Lyme Symptoms List for more.
Where Lyme disease is Occurring in the USA
- Lyme disease is being reported in every state, with an increased incidence in the North and North East, possibly due to climate change and warmer temperatures.
- 96% of cases have been reported in 13 states, including “… most states in New England, along with Virginia, Ohio, and Pennsylvania, and states across the northern Midwest, including Michigan, Illinois, Wisconsin, Minnesota, and North Dakota.” (Huffington Post)
- Over 17,000 cases of tick-borne diseases in Minnesota.
- Incidence in the Southern states is decreasing, possibly due to increasing populations of lizards, who do not transmit the disease to humans. This includes “Georgia, Louisiana, Mississippi, Tennessee, and Kentucky, … California, Oregon and Wyoming.” (Huffington Post)
- High-risk states include Wisconsin, Minnesota (parts), Illinois (parts), Pennsylvania (parts), New Hampshire, Maine, New York (parts), Maine, Rhode Island, Connecticut, New Jersey, Delaware, Maryland, and Virginia (parts).
Where Does is Occur Worldwide
80+ — Number of countries that the LDA (Lyme Disease Association) has found reported cases. The actual number of countries may be higher.
11 Steps for Avoiding the Disease and Resulting Co-Infections
This may be harder than we think as some experts believe most of the world’s population is already infected with the Borrelia spirochete. Lyme disease or co-infections can be dormant for years until some sort of trauma or other trigger occurs. Traumas and triggers include childbirth, car accidents, vaccines or stressful situations such as someone’s death, divorce, etc. (it can be passed on from mother to fetus.)
- Start with good nutrition, which increases the chances of being able to fight any associated infections.
- Maintain good health. This might seem obvious, but it needs to be said.
- Keep furry pets and especially kittens and puppies away from very young children. If you have no choice, at least make sure that children do not rub their faces in pet fur, and that pets do not lick or scratch your children.
- Reduce your time outdoors when ticks are most active in warmer weather, typically from April to September. Specifically, black-legged ticks are in wooded, brushy areas roughly from mid-May to mid-July.
- Wear repellent (e.g., DEET and Permethrin), especially if you spend a lot of time outdoors. The Minnesota Dept of Health says that products containing up to 30% DEET are safe for children and adults. Following manufacturer directions, Permethrin should not be used on your skin.
- Wear long-sleeved shirts and pants, with the latter, tucked into socks or boots. Light-colored clothes make it easy to spot ticks.
- See the Tick Management Handbook [http://www.ct.gov/caes/lib/caes/documents/special_features/tickhandbook.pdf] from the Connecticut Department of Public Health and Dr. Burrascano’s treatment guidelines [http://www.ilads.org/files/burrascano_0905.pdf].
- Check any gear or clothing that you bring back from infested outdoor areas. Dry clothes on high for an hour or more to kill ticks.
- Check your pets, and make sure they have adequate protection. This includes repellants and vaccines for their protection, but vaccines do not stop ticks from taking a ride into the home.
- If you have a yard, create a tick-safe zone by clearing tall grasses and bush at the perimeters, mowing the lawn frequently, stacking wood neatly, and disposing of old furniture and mattresses. Use pesticides as necessary.
- Talk to your doctor if you get a fever or rash.
Vaccines
While there was a vaccine, the CDC reports that the manufacturer discontinued it due to insufficient consumer demand. Anyone taking the vaccine before 2002 is likely no longer protected.
Related: